Bringing a newborn into the world can be an experience filled with awe and wonder, but can also bring about concerns and questions, especially when it comes to your baby's health. Like Jaundice for instance. Jaundice, a common condition in newborns, occurs when there is a buildup of bilirubin (explanation below, in the next few paragraphs) in the bloodstream due a change in baby's circulation. But did you know that continued breastfeeding plays a crucial role in supporting your baby through this phase? Rare is the case where the parents need to stop breastfeeding altogether or switch to complete supplementation with formula.
In the past few weeks I’ve met with too many parents that birthed their baby in a hospital setting who were misguided. Their breastfeeding journey was interrupted when they were told to supplement with formula instead of continuing to nurse at the breast. They were not shown that there are different options to supplementing i.e using lactation aids instead of giving the baby formula and sending the birth parent to pump. And doing so without the proper guidance. These parents are now having breastfeeding issues which I am helping support them through and hopefully resolve. Issues that would not have occurred if they were given the correct information or guided through this diagnosis of jaundice. In this blog post, we will explore why continuing to breastfeed is essential when your newborn has Jaundice.
When the baby continues to receive breast milk from the birth parent, this gives them adequate hydration in addition to the perfect nourishment and immune support they need. Breastmilk also acts as a mild laxative, helping the baby pass meconium (the thick, dark green stool) and bilirubin more efficiently.This can aid in reducing bilirubin levels and speeding up the resolution of Jaundice.
So what exactly happens when babies are born and why is there such a thing as Jaundice? And why are we so afraid of it?
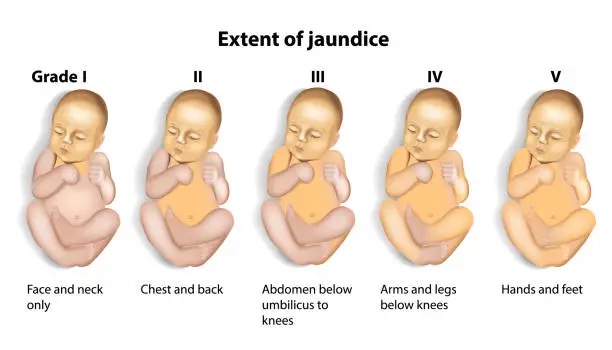
When babies are born, their circulation changes from fetal circulation to adapt to being earthside. Their red blood cells break down rapidly and inside the heme component there is a substance called bilirubin (billy-roo-bin). This is a yellow pigmented antioxidant that protects newborns in their extra uterine life and adapts to all the oxygen they are now exposed to. This is a normal occurrence, but when the liver (due to its immaturity) is not keeping up with the pace of clearing this accumulation, it causes the skin and white part of the eye (sclera) to look yellow. This unconjugated (fat soluble) bilirubin is escorted by albumin to the liver where it is turned to conjugated bilirubin (making it water soluble). After this process is done, bilirubin is secreted to the bowels where it is turned into urobilinogen and can be eliminated in the baby's poop (medical term ;)). Some small amount of urobilinogen will get reabsorbed back into the bloodstream from the gut, and will then be excreted in the urine. This is a simplified description of what happens in the baby's body.
It is the buildup of bilirubin levels in the bloodstream that causes alarm, because if there are truly high levels of this substance and it crosses the blood brain barrier, then it can accumulate in the brain, causing Kernicterus aka bilirubin encephalopathy. This usually occurs with levels of 25 mg/dl of bilirubin and greater.
So again, it all comes down to finding the root cause of what’s causing the elevation.
It could be from increased levels of unconjugated bilirubin (like from rapid breakdown of red blood cells - hemolysis or birth trauma; cephalhematoma-bruising on the head, or any other type of bruising, ABO incompatibility etc.) or from the lessened ability to eliminate the bilirubin (like low levels of albumin, the protein that transport the bilirubin to the liver to get conjugated or an obstruction in the biliary system).
In most cases, the reason why the bilirubin levels increase is because babies are NOT getting enough breastmilk. So why not focus on helping the family how to breastfeed more efficiently? Make sure that the latch is perfect and the baby can then transfer milk from breast more efficiently. Why not encourage more skin to skin, less swaddling the baby so tight that you may miss a feeding session? Why not show the family that if supplementing is absolutely necessary it can be done with an SNS (supplementing nursing system), or cup feeding? Why can’t we encourage supplementing with mother’s expressed milk or even donor milk until the lactating parent can make enough to answer the demand?
We CAN! It’s just easier not to. It’s easier to give a bottle with formula, because we’ve normalized this. But the shift that needs to happen is to normalize all the things I mentioned before.
Breastfeeding is not only the perfect nourishment for your newborn but also a vital tool in managing jaundice. By providing hydration, immune support, and comfort, breast milk can play a significant role in helping your baby recover from this common condition. Consult with your healthcare provider and a lactation consultant for guidance and support during this journey. Don’t be afraid to ask the questions, request options that may not be the mainstream in your birth setting. With patience, perseverance, and the power of breast milk, you and your baby can navigate Jaundice together and continue to nurture the beautiful bond that is growing between you.

What to look for to make sure that you and your baby are on the right path?
I hope this information was helpful and reassuring for you!
Credits:
https://ibconline.ca/information-sheets/breastfeeding-and-jaundice/
https://www.nhs.uk/conditions/jaundice-newborn/causes/
https://www.ncbi.nlm.nih.gov/books/NBK559120/
https://www.cdc.gov/breastfeeding/breastfeeding-special-circumstances/maternal-or-infant-illnesses/jaundice.html
https://babychildandco.com/all-you-need-to-know-about-newborn-jaundice/